EHR integration testing ensures healthcare systems work together without errors that could impact patient safety or compliance. The process is complex, with challenges like data validation, regulatory requirements, and system interoperability. Testing teams often face:
- Data risks: Errors in patient data (e.g., missing fields, invalid codes) can disrupt care.
- Compliance hurdles: Adhering to HIPAA, GDPR, and FDA standards requires detailed checks.
- Interoperability issues: Systems must follow protocols like HL7/FHIR for smooth communication.
- Time constraints: Tight deadlines often lead to rushed validations, increasing risks.
Effective strategies include reactive methods (fixing issues after they occur), proactive measures (preventing errors upfront), and automated testing frameworks (streamlining repetitive tasks). Balancing these approaches ensures safer, more reliable integrations while meeting technical and regulatory standards.
EHR System 2026 LIS|LAB Integration Project: Your Complete Implementation Guide #ehrintegration #hl7
sbb-itb-e3aed85
1. Reactive Error Handling Methods
Reactive error handling comes into play after a problem arises during EHR integration. For example, if a pharmacy system sends a prescription to an EHR and encounters an invalid NHS number, the system must quickly identify the issue and provide clear feedback. This is where standardized error reporting becomes crucial. Using FHIR's OperationOutcome resource, systems can include detailed diagnostics, error codes, and severity levels to explain why the transaction failed.
Error Scenario Coverage
Testing teams must anticipate various failure points. Here are a few common ones:
- Identity validation failures: These occur when patient, practitioner, or organization records are missing from the database.
- Security denials: These happen when patients haven't given consent for data sharing or when organizations lack the necessary permissions.
- Malformed requests: Errors arise due to issues like malformed JSON or XML, missing mandatory headers (e.g., interaction IDs), or incorrect HTTP verbs (e.g., using POST instead of GET).
- Resource validation errors: These occur when submitted data doesn't align with FHIR profiles or references non-existent resources. For instance, one hospital's interface rejected all lab results for a day because a required
statusfield was missing, causing the FHIR server to block every message.
These scenarios highlight the importance of robust validation mechanisms, which are discussed in detail below.
| HTTP Code | Issue Type | Example Error Code | Description |
|---|---|---|---|
| 400 | value | INVALID_NHS_NUMBER | The supplied NHS number is invalid |
| 404 | not-found | PATIENT_NOT_FOUND | Patient record does not exist on the server |
| 403 | forbidden | NO_PATIENT_CONSENT | Patient has not provided consent for sharing |
| 422 | invalid | REFERENCE_NOT_FOUND | A FHIR reference in the request is missing |
| 504 | transient | GATEWAY_TIMEOUT | A downstream server timed out during the request |
Data Integrity Validation
Once potential error scenarios are identified, rigorous data validation becomes the next step. Validation errors can impact 5%–10% of incoming FHIR resources. Reactive methods safeguard data integrity by applying multiple layers of validation:
- Structural checks: Ensure JSON or XML syntax is correct.
- Cardinality checks: Verify that required fields (e.g.,
Observation.status) are included. - Value domain constraints: Confirm that formats like dates or numeric types are accurate.
- Terminology bindings: Validate coded fields (like ICD-10 or SNOMED codes) against predefined ValueSets to reject invalid entries before they affect clinical records.
MedKit highlights the delicate balance required in validation:
Deciding how much validation to do in production is a careful decision: too little and you risk bad data, too much and you risk missing data.
Interoperability Testing
To complement error detection and validation, interoperability tests are essential for ensuring system resilience. Negative testing deliberately introduces invalid data, unauthorized access attempts, and incorrect message formats to confirm that error-handling mechanisms respond as expected. During HL7 unit testing, developers implement exception-handling logic before handing the system over to QA. Shreekant Majge from Radiology Partners Inc underscores the importance of thorough testing:
Regression testing identifies unexpected differences in data mapping between staging and production environments, preventing errors that could delay patient treatment.
Additionally, HL7 smoke tests, which typically take 4–6 hours, verify basic interface functionality before moving on to more comprehensive testing.
2. Proactive Error Handling Methods
Proactive error handling focuses on addressing potential issues before they arise by validating input data prior to transmission. This approach is especially relevant, as 70% of early FHIR projects encounter missing elements or invalid code values during initial testing phases, emphasizing the importance of early validation efforts.
Error Scenario Coverage
Anticipating failure scenarios is key to building resilient systems. Test teams should create cases that simulate negative conditions, such as invalid data inputs, unauthorized access attempts, or incorrect message formats. These tests ensure the system can manage errors effectively. Every documented requirement should align with a test case, and scenario-based testing - like linking patient registration to billing systems - can reveal issues that might otherwise disrupt clinical workflows. This approach helps identify problems before they affect patient care.
Data Integrity Validation
Proactive validation uses multiple layers of checks to ensure data integrity before it even reaches the server. Unlike reactive methods that address errors after they occur, proactive measures enforce business rules and standardize data translation upfront. For example, reactive validation might reject an entire patient record due to one invalid field, leading to significant data loss. Proactive validation avoids this by applying invariants to enforce rules, leveraging interface engines for consistent data translation, and using central data dictionaries to standardize terms - like mapping "HbA1c" to "Hemoglobin A1c" - across systems.
Interoperability Testing
Early detection of integration issues is possible through proactive interoperability testing. Automated tools like Postman or REST Assured can validate data structures, content, and error responses in real time. Additionally, mimicking production environments - hardware, network configurations, and software setups - ensures testing outcomes align with actual performance.
Regulatory Compliance
Proactive error handling also strengthens compliance efforts, particularly for regulations like HIPAA. Measures such as end-to-end encryption (AES-256 for stored data and TLS 1.3 for data in transit) protect sensitive patient information from security breaches. When using production data for testing, techniques like de-identification or masking are vital to maintaining compliance. Furthermore, audit trails and automated alerts allow teams to identify and resolve data flow interruptions before they escalate into patient care issues or regulatory violations.
3. Automated Testing Frameworks
Automated testing frameworks play a key role in improving error detection and system resilience. By streamlining EHR integration testing, these frameworks ensure that error handling and data recovery meet strict regulatory and patient safety standards. When incorporated into Continuous Integration/Continuous Delivery (CI/CD) pipelines, they provide quick feedback on how system updates impact existing error-handling processes, helping to catch issues early in development.
Error Scenario Coverage
Automated frameworks are particularly effective for negative testing, where systems are intentionally exposed to invalid data, unauthorized access attempts, or incorrect message formats. This approach ensures systems handle errors gracefully and removes human subjectivity from the process. Scripts use assertion-based checks to confirm the system responds with appropriate HTTP codes, such as 4XX or 5XX errors, when invalid operations occur.
These tools also simulate external systems - like labs or pharmacies - using actor-based models to test how the system handles external failures. Dynamic variable substitution allows scripts to run seamlessly across environments without reconfiguration. Additionally, synthetic data generation creates scenarios involving rare clinical conditions or unusual workflows that real patient data can't replicate. Together, these methods enhance both reactive and proactive error-handling strategies.
Data Integrity Validation
Automated frameworks assess data integrity by checking for completeness (missing values), conformance (correct format and type), plausibility (values within acceptable ranges), and consistency (agreement across systems). For example, among automated Data Quality Assessment programs, 15 focus on completeness, while 12 address value conformance. These frameworks can handle large EHR datasets quickly, far beyond the capacity of manual testing.
Tools like Postman and ReadyAPI validate API message structure and content, while healthcare-specific tools such as Touchstone and IHE Gazelle test FHIR and HL7 conformance. Automated scripts also include teardown procedures, ensuring servers are reset to clean states after testing, ready for subsequent runs.
Interoperability Testing
Specialized tools within automated frameworks address challenges across the three levels of interoperability: foundational, structural, and semantic. For instance, the NIST Electronic Prescribing (eRx) Validation Tool evaluates systems for ONC Health IT Certification, while the NIST Edge Test Tool (ETT) checks transport protocols and message specifications for secure data exchange. The FHIR TestScript resource provides executable documentation, enabling automated systems to verify conformance without being tied to specific implementations.
"Standards based systems are the foundation for achieving this goal. However, standards alone are not enough to ensure this promise; conformance and interoperability testing are essential".
Regulatory Compliance
Automated frameworks support regulatory compliance by using synthetic data generation and automated de-identification tools, reducing the need for real patient data during testing. They also create detailed audit trails and documentation to ensure compliance with privacy regulations. By delivering consistent and repeatable safeguards, these frameworks help mitigate risks such as system outages, security breaches, and errors that could jeopardize patient safety, like delayed diagnoses or medication mistakes. Experts recommend dedicating 15–20% of the EHR integration project budget or timeline to thorough testing, underscoring its critical role in avoiding integration failures.
Advantages and Disadvantages
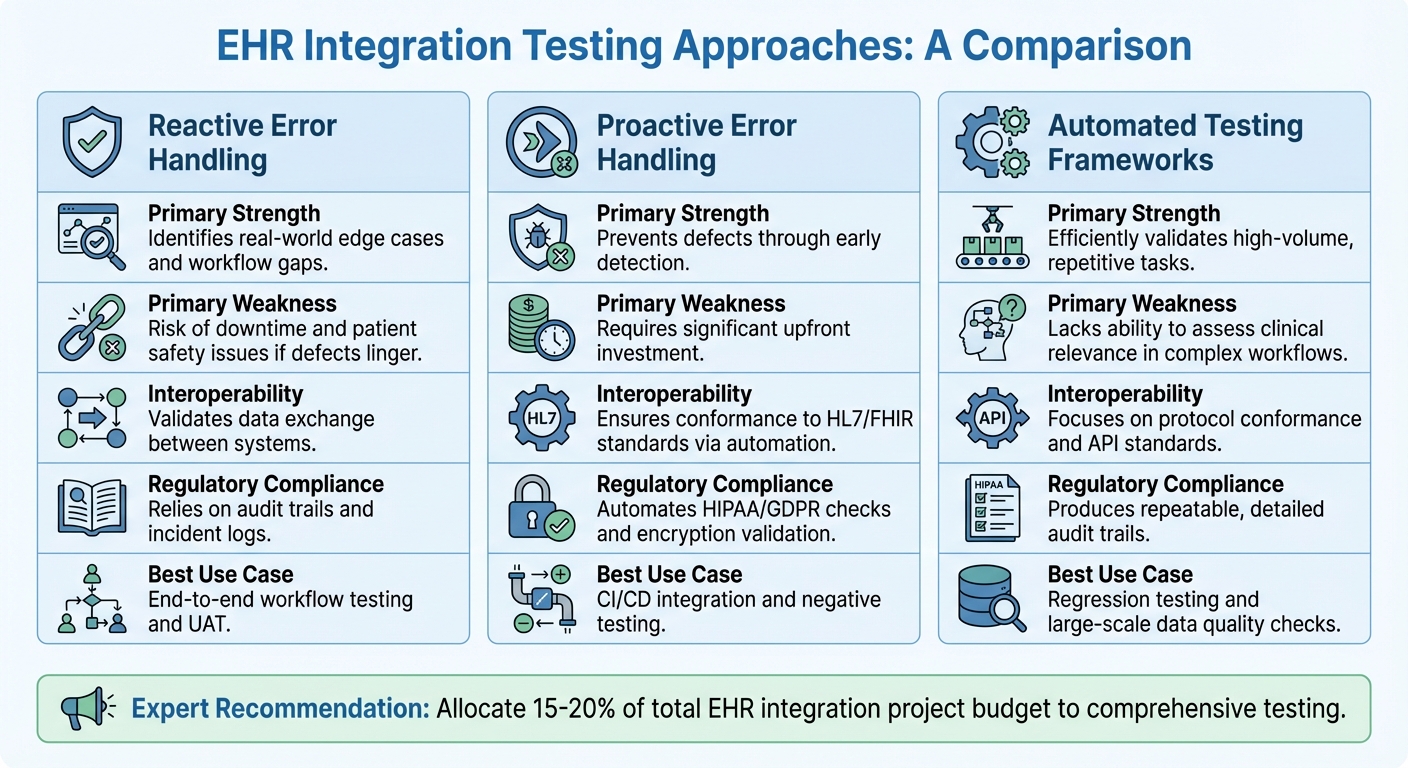
EHR Integration Testing: Comparing Reactive, Proactive, and Automated Approaches
Let’s take a closer look at the pros and cons of different error-handling strategies when it comes to managing EHR integration testing. Each approach has its own strengths and weaknesses, and understanding these trade-offs is key to building a well-rounded testing strategy.
Reactive error handling is great for uncovering edge cases that only surface in real-world scenarios. This method shines during end-to-end testing, especially in areas like patient class mapping. However, the downside is that issues are only identified after they’ve already caused disruptions. Risks like medication errors, delayed diagnoses, or compromised patient safety are real concerns here. Since this approach depends on audit logs and post-incident fixes, it often means problems are addressed only after they’ve impacted operations.
On the other hand, proactive error handling focuses on preventing defects before they occur. Techniques like CI/CD and unit testing catch issues early, long before they hit production. Ganesh Varahade, Founder & CEO of Thinkitive Technologies, highlights its benefits:
Automated testing in healthcare integration ensures systems are error-free, reliable, and compliant. It accelerates testing cycles, detects bugs early, reduces manual effort, and improves data accuracy and security.
But let’s not ignore the challenges. Proactive methods demand a significant upfront investment in tools and modular scripts. These scripts also need constant updates whenever EHR vendors modify their API specifications, adding to the ongoing workload.
Then there’s automated testing frameworks, which excel at repetitive validation tasks. They’re particularly effective for technical conformance testing, such as ensuring HL7/FHIR standards are met. While they offer speed and efficiency, they can’t fully replace clinical oversight. For example, during User Acceptance Testing (UAT), clinicians still play a critical role in validating workflows and ensuring patient safety.
Experts suggest that 15–20% of the total EHR integration project budget should go toward comprehensive testing. Meeting technical performance benchmarks - like 99.9% uptime, response times under 2 seconds, and error rates below 0.1% - often requires a mix of these approaches rather than relying on just one.
Here’s a quick comparison of the three methods:
| Feature | Reactive Error Handling | Proactive Error Handling | Automated Testing Frameworks |
|---|---|---|---|
| Primary Strength | Identifies real-world edge cases and workflow gaps | Prevents defects through early detection | Efficiently validates high-volume, repetitive tasks |
| Primary Weakness | Risk of downtime and patient safety issues if defects linger | Requires significant upfront investment | Lacks ability to assess clinical relevance in complex workflows |
| Interoperability | Validates data exchange between systems | Ensures conformance to HL7/FHIR standards via automation | Focuses on protocol conformance and API standards |
| Regulatory Compliance | Relies on audit trails and incident logs | Automates HIPAA/GDPR checks and encryption validation | Produces repeatable, detailed audit trails |
| Best Use Case | End-to-end workflow testing and UAT | CI/CD integration and negative testing | Regression testing and large-scale data quality checks |
Conclusion
Integrating EHR systems effectively requires a blend of reactive and proactive testing methods. On the reactive side, handling network timeouts and issuing immediate clinical alerts through standardized FHIR OperationOutcome responses ensures timely issue resolution. Proactive strategies, meanwhile, help prevent challenges like duplicate records, mapping errors, and data corruption from reaching production environments.
To tackle specific error scenarios, healthcare teams need tailored approaches. For instance, duplicate HL7 messages can be managed with proactive idempotency keying, using the MSH-10 field as a primary key to collapse replays within a 7–30 day timeframe. When dealing with endpoint timeouts, reactive retries with bounded exponential backoff ensure eventual delivery without overloading systems. Additionally, proactive message comparison testing - running production HL7 messages in a staging environment to compare outputs - can identify mapping issues early, avoiding clinical disruptions.
Budget allocation plays a pivotal role in ensuring comprehensive testing. Teams should focus on automating high-risk areas like patient data exchange and medication orders. Using synthetic or de-identified data allows for testing edge cases without compromising HIPAA compliance.
These strategies emphasize the importance of aligning technical solutions with clinical workflows.
"The root problem is that most teams treat EHR integration like a standard API connection when it's actually clinical workflow design disguised as a technical project."
Start with a minimum viable integration that delivers tangible clinical value and gradually expand testing coverage. Involve clinicians throughout the process - not just during User Acceptance Testing but also during the design of testing protocols. This ensures that HL7/FHIR technical standards align with real-world clinical needs. Aim for benchmarks like 99.9% uptime, response times under 2 seconds, and error rates below 0.1%. Meeting these targets directly impacts patient care, making healthcare delivery safer and more efficient.
FAQs
How do I choose between reactive, proactive, and automated testing?
When selecting a testing approach for EHR integration, it’s all about your goals. Let’s break it down:
- Reactive testing deals with problems after they happen. While this might work in some fields, in healthcare, it’s risky. Data accuracy and patient safety are at stake, making this approach less than ideal.
- Proactive testing takes a preventive approach. It emphasizes planning and thorough validation to catch potential issues before they arise.
- Automated testing brings efficiency to the table. It allows for continuous performance checks, ensuring the system runs smoothly over time.
For healthcare, blending proactive and automated testing is often the best route. This combination helps reduce risks and maintain reliability in such a critical environment.
What’s the fastest way to catch HL7/FHIR mapping errors before go-live?
The fastest way to spot HL7/FHIR mapping errors before going live is by using validation tools and following mapping guidelines. These tools help catch problems such as formatting issues or missing fields early in the process, making integration much easier. By using HL7 FHIR validation tools, you can simplify the workflow and minimize the chances of major errors during deployment.
How can we test with realistic data without violating HIPAA?
You can maintain HIPAA compliance by leveraging synthetic datasets. These datasets are designed to imitate the complexity of actual clinical data but without exposing any real patient information. This approach allows for safe and comprehensive testing without risking privacy breaches.
To ensure compliance, it's essential to follow key best practices:
- Encrypt data to protect it from unauthorized access.
- Enforce strict access controls to limit who can view or handle sensitive information.
- Use secure APIs to prevent vulnerabilities during data transmission.
Additionally, hybrid models offer another layer of protection. By keeping sensitive data stored on-premises and conducting testing in tightly controlled environments, you can further reduce risks while still achieving your testing goals.

